While this saga is not yet complete, I feel compelled to share it with you. Not because I want you to do anything, rather because you may be in the same boat. I’m sharing my journey. Do not take this as financial or medical advice.
Obamacare was supposed to make certain insurance companies actually paid for some things. Like all government plans, the schlocky ones have found ways to screw with you. I’m not the first to write about this nor will I be the last. Here is a good link to some facts. It is where the following screen scrape comes from.
Even if you call your insurance company ahead of time they are probably going to lie to you. I know mine did. I called. They had my history and I was told I was covered if I used their provider. I did. Now I’ve got about $3K in bills. Insurance paid for nothing. They just had “negotiated discounts.”
The scam being run right now is to classify all colonoscopies as either diagnostic or “monitoring.” The insurance company passes all bills to you and applies it against your deductible.
When I got my first $900+ bill from the service provider I assumed I had the typical shit insurance Illinois is famous for. I paid the bill. Then I thought more about it. After that I got a $900+ bill from the anesthesiologist. Today, I got another $1500+ bill from the service provider. Why did I call to find out if it would be covered? Because I had already searched on-line via “Cheap Colonoscopy” and found this:
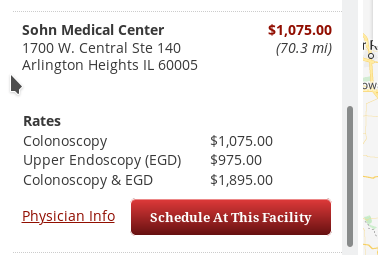
Paying with cash/plastic involving no insurance company what-so-ever, the price was $2K to do both upper and lower. If you’re already knocked out you might as well get both done.
I called Health Alliance after I got the anesthesiologist bill to find out what was going on. That’s when I was told
“It wasn’t billed as a screening. Had it been billed as a screening it would have been covered. Call your doctor.”
Of course calling the doctor and getting the billing department and telling them they were supposed to bill as a screening only to be told
“We hear that a lot. We cannot bill it as a screening because you had polyps removed during your 2012 colonoscopy.”
So, I opened a complaint with IDOI (Illinois Department of Insurance). I didn’t expect much and wasn’t disappointed. They forwarded the complaint to the company and allowed the company to say it was “monitoring” even though I had no polyps this time. They closed the case.
Then I went to the healthcare.gov site and called 1-800-318-2596. I spoke with an incredibly helpful woman who put me on hold to check with their support people who are well versed in what is and is not supposed to be covered. A bit later she came back on the line and told me
“Write down this number. 888-866-6205. When you get through the menu request an External Review Request Form. Fill it out and fax it along with all of the documentation to the fax number on the form. They have to pay for one every so many years no matter what and your last one was in 2012.”
Armed with my new knowledge I filed another document with the IDOI informing them this was an exchange purchased policy and according to the people working at the exchange insurance had to pay for one every so many years no matter what. Honestly I expect the same result.
I called the 888 number and danced through the menu. Ended up having to leave a message. About 4:30 the following day I got a voice mail from a very helpful girl working for Maximums Federal Services. She emailed me the form and stayed on the line to be certain it got through. She informed me there is a time limit which she didn’t have the exact length of, but to fill everything out and fax it all to the number. She also informed me of the rules.
- You have to have documented an internal review request. This means you have to have something in writing from the insurance company indicating you requested they cover the expense and them denying. Phone calls won’t be of much use.
- You can only request an external review after you have exhausted your internal review options.
- They need all of the documentation, otherwise the review will be performed based on what the insurance company cares to share with them.
- There is a time limit of some number of months.
Number one is where people really screw up. Talking with an insurance company on the phone gives you no paper trail. Your department of insurance (or director of insurance as some places call them) should have a nice Web site where you upload documents and the documents the insurance company sends get loaded.
Many people don’t know their state has a department/director of insurance. You have to exhaust that option too.
Number 4 is the real killer. It generally takes a month after services being rendered before the first bill arrives. If you take the bait and play the “ask your mother, ask your father” game the insurance company spins you around with, telling you to get your service provider to re-bill, having them tell you they have to bill it the way they billed it, etc. You can easily burn another month. I made the phone calls to each only once.
The game is time. If they manage to make you chase your own tail for however many months the limit is, they win. You cannot get an external review.
How many of you even knew there is an External Review Process for ACA plans? I didn’t. The number and the information aren’t on the healthcare.gov site. I imagine the phone number changes every so often if the work is contracted out but you won’t find it on the site.
Don’t just jump to the number. You have to exhaust all other options first.
I don’t yet know how this turns out. From the conversation I had with the very helpful person, it sounds like they are aware of insurance companies trying to skip out on paying for colonoscopies by getting them billed under other codes.
This is my journey to date. I’m sharing it with you in case you happen to be walking down the same road without a map.

